Description
Clinical History
A 22-year-old male presented with a 2-week history of generalised malaise, weight loss and bruised skin without any trauma. He recently developed 5 days of productive cough and fevers. He was admitted to hospital for further investigations but had a sudden loss of consciousness and died a few minutes after admission to hospital.
Pathology
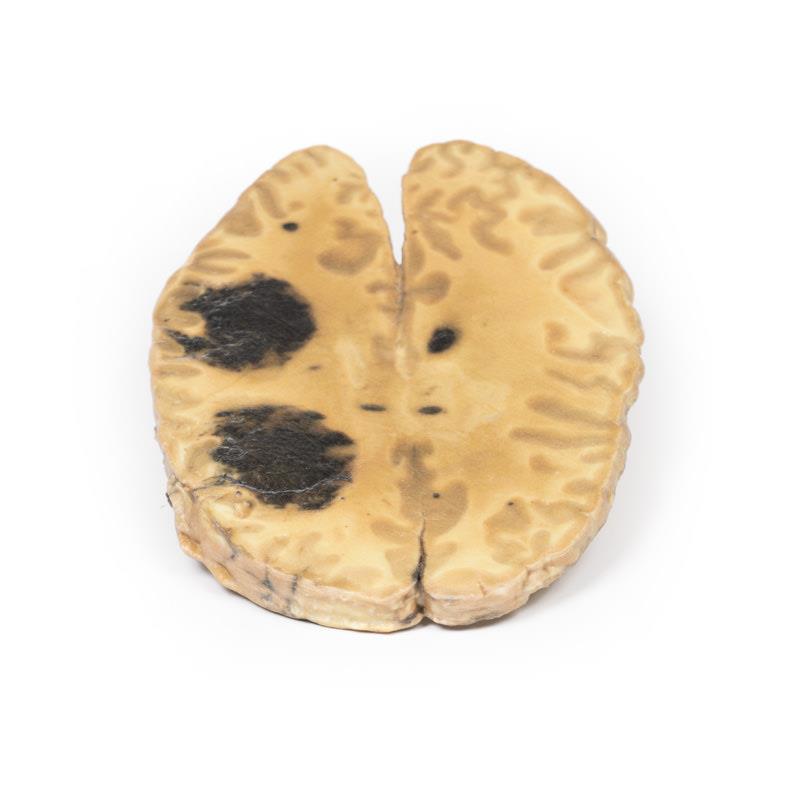
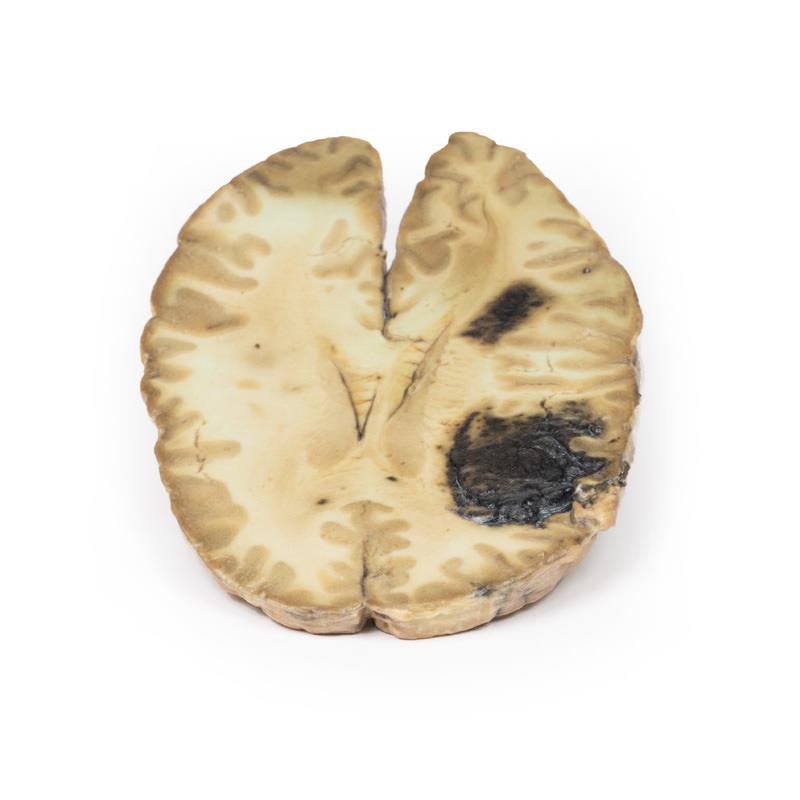
The specimen is a horizontal slice of brain displaying the superior cut surface. In the right frontal and parietal regions are two large intraparenchymal haemorrhages each 5 cm in maximum diameter. Several smaller haemorrhages are present in the white matter of both hemispheres. This is an example of multiple intraparenchymal cerebral haemorrhages in a patient with acute myeloid leukaemia (AML).
Further Information
Intraparenchymal brain haemorrhages are a result of small, ruptured vessels within the brain causing haemorrhage. They are usually associated with sudden onset neurological symptoms. The most common causes for spontaneous (no-traumatic) intraparenchymal hemorrhages are hypertension and cerebral amyloid angiopathy with a peak incidence in the 6th decade of life.
AML is a cancer of haematopoietic progenitors causing bone marrow failure, due to immature blast cell accumulation in the marrow. The immature blasts affect the production of other bone marrow-derived cells leading to bone marrow failure causing anaemia (decreased erythrocytes), thrombocytopaenia (decreased platelet production and a haemorrhage tendency) and neutropenia (decreased neutrophil production). These in turn lead to a wide spectrum of disease complications, which have to be anticipated and managed. Infection is the leading cause of death in AML as a result of neutropenia. Intracranial haemorrhage is the second most common cause of death in AML, due to low or dysfunctional platelets caused by the thrombocytopaenia. A severe form of haemorrhage is termed disseminated intravascular coagulation (DIC) is common in AML. DIC is characterised by small blood clots developing throughout the bloodstream, blocking capillaries. The increased clotting depletes the platelets and clotting factors needed to control bleeding, causing excessive bleeding.
Symptoms depend on the location and severity of the bleed. Interventions include surgical evacuation of the haematoma, reversal of the coagulopathy, treatment of any seizures, and regulation of the intracranial pressure. Interventions are dependent on the severity of the bleed and clinical context. The 30-day mortality for intracerebral haemorrhage ranges from 35-50% with most deaths occurring in the first 48 hours.