Description
Clinical History
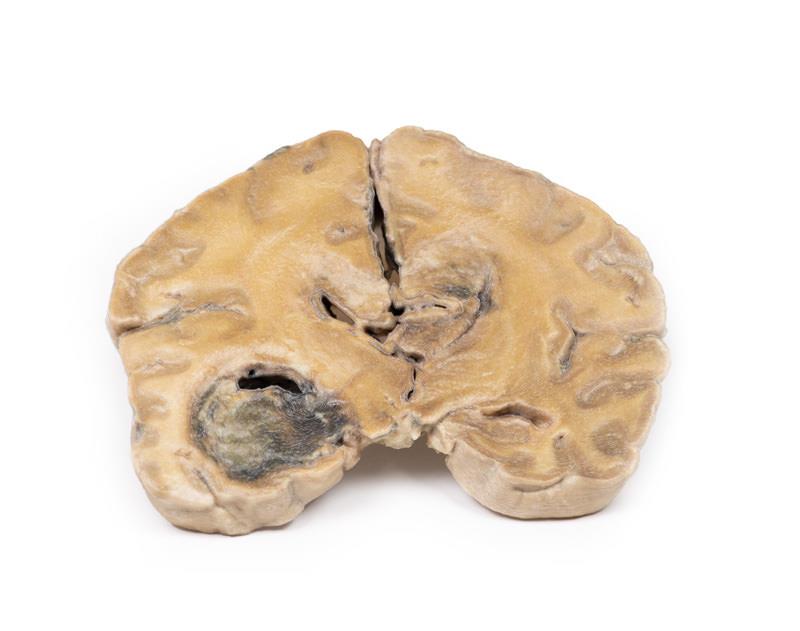
Over a 3-year period, a 57-year-old woman had intermittent frontal headache and memory disturbance with progression to psychiatric disturbance, and ultimately vomiting and meningeal signs. Localising neurological signs only developed late in the course of the disease.
Pathology
Coronal section through the cerebral hemisphere demonstrates a round, haemorrhagic, variegated tumour in the left temporal lobe. Less well-defined tumour tissue extends across the mid-line replacing the corpus callosum. The ventricular system has been almost totally obliterated. Further sections through the cerebral hemisphere confirmed that these apparently separate lesions are extensions of one massive tumour.
Further information
Gliomas are the second most common cancer of the central nervous system after meningiomas. The term “glioma” refers to tumours that are histologically similar to normal glial (macroglial) cells* i.e. astrocytes, oligodendrocytes and ependymal cells. They arise from a progenitor cell that differentiates down one of the cell lines. GBMs can arise in the brain “de novo” or evolve from lower-grade astrocytomas or oligodendrogliomas. GBM is often referred to as a grade IV astrocytoma. They are differentiated histologically from anaplastic astrocytomas by necrotising tissue surrounded by anaplastic cells as well as by the presence of hyperplastic blood vessels.
GBMs are more common in males. It is most commonly diagnosed in the 6th decade of life. Genetic risk factors include neurofibromatosis type 1 and Li-Fraumeni syndrome. Previous brain radiotherapy is also associated with increased risk of GBM. Symptoms vary depending on the location of the GBM, but may include any of the following:
• Persistent headaches
• Double or blurred vision
• Vomitng
• Loss of appetite
• Changes in mood and personality
• Changes in ability to think and learn
• New onset of seizures
• Speech difficulty of gradual onset
Diagnostic tools include computed tomography (CT scan) and magnetic resonance imaging (MRI). Around 50% of these tumours occupy more than one cerebral hemisphere. GBMs commonly extend into the ventricular walls or meninges, and thus into the central spinal fluid (CSF). Spinal cord spread is uncommon. Metastasis beyond the central nervous system is rare. Tumour growth causes cerebral oedema leading to increased intra-cranial pressure. These are biologically aggressive tumours, and if left untreated survival is typically 3 months. The mainstay of treatment for GBMs is surgery, followed by radiation and chemotherapy.
*Microglia are a different lineage from macroglia. The former are related to the macrophage lineage, and arise initially from the yolk sac and later in development from the bone marrow.