Description
Clinical History
A 45-year old male presented with a lump in his left supraclavicular area. The swelling had been increasing in size over 6 months. Excision biopsy of the lump showed Hodgkin lymphoma (HL). Ten months later he was readmitted with left shoulder pain and swelling of his left arm. Examination revealed generalised lymphadenopathy with significant swelling in his left supraclavicular and axillary regions. He was treated with radiotherapy and Thiotepa chemotherapy. He developed vomiting. A subsequent barium meal showed duodenal obstruction from extrinsic lymph node compression. He continued to deteriorate and died 2 weeks after readmission.
Pathology
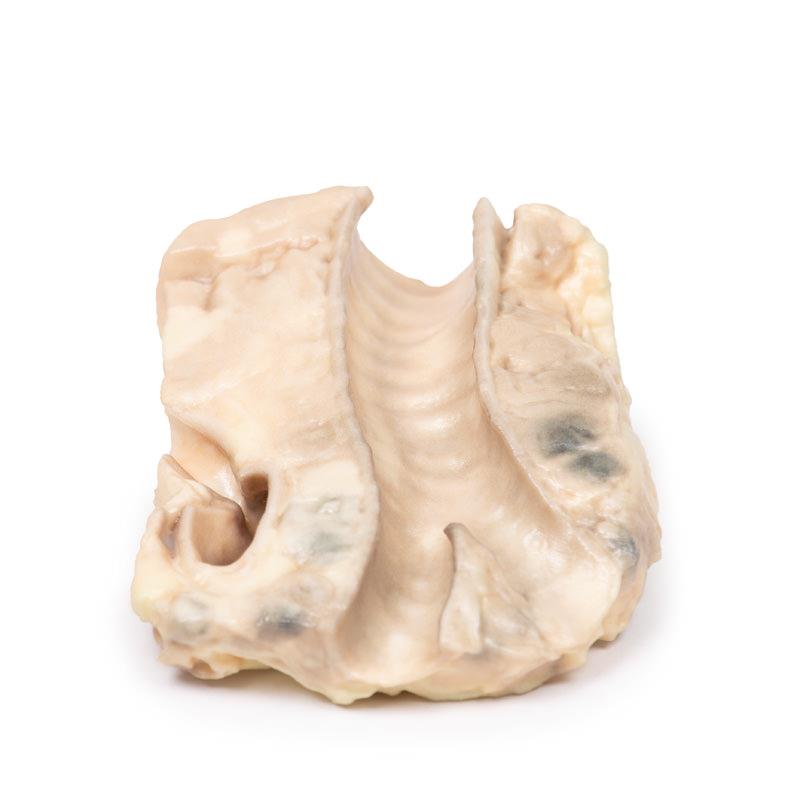
The 3D print shows the tracheal bifurcation with adjacent para-tracheal and peri-bronchial lymph nodes. The trachea has been opened longitudinally and is viewed from behind. The para-tracheal lymph nodes are pale and matted (fused) together. Similar abnormal tissue is seen as a confluent pale mass on the left side of the trachea, above the aortic arch, which is seen cut in cross-section as a void space with branches arising. The peri-bronchial lymph nodes are also enlarged, and contain carbon pigment. The circumscribed small paler areas in the lymph nodes and extra-nodal tumour are foci of necrosis. There is an atheroma in the wall of the aorta but it is difficult to see in the 3D print.
Further Information
Hodgkin Lymphoma (HL) is a malignancy of lymphocytes. It is characterised by the presence of neoplastic giant cells called Reed Sternberg cells. There are 5 main subtypes according to the WHO Lymphoma Classification, based on the morphology, immunophenotyping and genetics. Activation of the transcription factor NF-kB is a common pathway of tumorigenesis among the subtypes. This promotes proliferation, reduces apoptosis, and induces expression of cytokines that recruit the immune cells that surround Reed Sternberg cells in HL.
There is a bimodal age distribution with a peak in late adolescence/early adulthood and a second peak in older adults. HL accounts for just under 1% of all cancers worldwide. Infection with Epstein Barr Virus (EBV) contributes to the pathogenesis of the main subtypes of HL. The viral genome causes genetic alterations that lead to aberrant signal pathways, although the precise mechanism is not known. Immunosuppression (e.g. HIV infection or post- organ transplant) and positive HL family history are also risk factors. HL commonly presents as painless lymphadenopathy, pruritus, weight loss, fevers and night sweats. Later disease sees organ spread to the spleen, liver and bone marrow. Compressive symptoms can arise from enlargement of lymph nodes and infiltrated organs. HL is diagnosed with staging CT scan, excision biopsy of involved nodes and bone marrow biopsy. Treatment involves radiotherapy and chemotherapy. Although previously incurable, the overall survival of HL has improved significantly over the last 5 decades as a result of modern therapies: diagnosed at an early stage, it is almost 90%, and even later stage disease has a favourable prognosis.