Description
Clinical History
A 50-year-old alcoholic was admitted with a 2-week history of weakness and shortness of breath. At the onset of the illness he reported a productive cough, chest pain and blood-stained sputum. Examination revealed a febrile, cyanosed, drowsy man with grunting respiration. A friction rub was present over the right lower lobe. The remainder of the examination was unremarkable. The patient steadily deteriorated and on the morning of his death, a lumbar puncture was performed. Green opalescent fluid was obtained. A blood culture grew Streptococcus pneumoniae.
Pathology
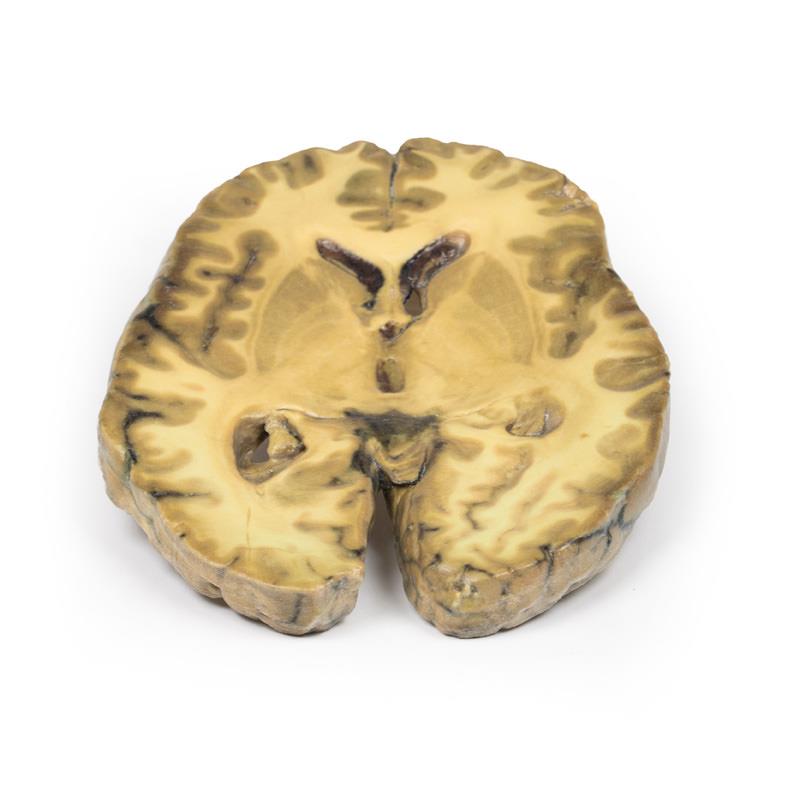
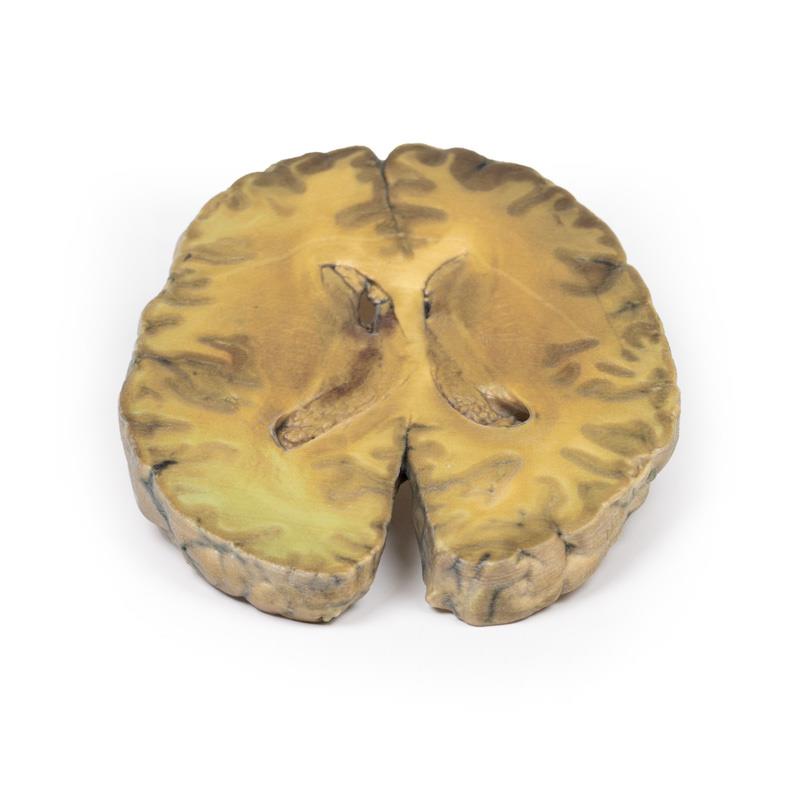
This specimen is an example of ventriculitis, with pneumococcal meningitis and right basal pneumonia also being found at autopsy. The horizontal slice through both cerebral hemispheres displays both of the lateral ventricles. The ventricles show a thickened, rough ependymal lining with cellular debris accumulation around the choroid plexus and also in the anterior horn. The lower surface shows similar changes and also displays the normal arrangement of the caudate nucleus, lentiform nucleus and internal capsule.
Histology demonstrated extensive infiltration of neutrophils in the sub-arachnoid space as well as multifocal severe (sub)endothelial infiltration with obstruction of vascular lumen and involvement of the blood vessel walls. The inflammation extended into the cerebral parenchyma causing haemorrhage and necrosis.
Further information
Ventriculitis is an uncommon complication of intracranial infection. In adults, it more commonly occurs as a secondary complication of surgical intervention / instrumentation or trauma, rather than from primary community-acquired meningitis. In these cases, causative organisms are similar to other nosocomial (hospital-acquired) infections, in particular staphylococci or resistant Gram-negative bacilli. Neonates aged less than 6 months have a higher incidence of ventricular infection. Presentation may be more subtle than in bacterial meningitis or may be as obstructive hydrocephalus, secondary to resulting aqueductal obstruction. Diagnosis is dependent on laboratory CSF testing and imaging, in particular using CT scans and MRI. Prolonged intravenous antibiotic therapy is a mainstay of treatment with consideration to achieving effective concentrations in CSF and brain tissue